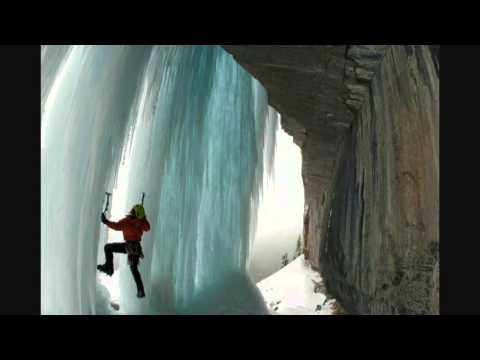
Title: Climbing out of addiction and depression Margo Talbot at TEDxCanmore
Channel: TEDx Talks
Climbing out of addiction and depression Margo Talbot at TEDxCanmore by TEDx Talks
depression from drug use, depression from drug abuse, depression after drug use, depression symptoms drug use, depression injecting drug users, depression and drug use statistics, can drugs cause depression
Drug-Induced Depression: Shocking Truth You Need to Know!
Drug-Induced Depression: Unveiling the Unexpected
Have you ever considered the medications you take could be silently impacting your mental state? It's a complex relationship, but one that warrants attention. We often focus on the benefits of pharmaceuticals. However, there's a darker side that deserves acknowledgement. This article delves deep. It explores a truth that some may find unsettling: drug-induced depression. Prepare yourself for some surprising revelations.
The Silent Culprit: How Medications Can Trigger Despair
Many medications can trigger depressive symptoms. This potential side effect often goes unnoticed. The connection can be subtle. It may appear gradually. Or, it may hit you like a ton of bricks. The very drugs designed to heal can sometimes inflict hidden suffering. The process isn't always straightforward. Several factors play a part. Patient's individual biology is pivotal. The dosage of the medication also matters. Moreover, pre-existing mental health conditions can increase the risk. Therefore, it is crucial to stay informed.
Common Offenders: Medications That May Surprise You
Certain types of medications are more likely to induce depression. It's not an exhaustive list. However, it highlights the range of potential culprits. Consider these categories carefully.
- Blood Pressure Medications: Some antihypertensives are implicated. Beta-blockers, in particular, have been linked. They block the effects of adrenaline. This may indirectly affect mood.
- Hormonal Treatments: Birth control pills and hormone replacement therapy can sometimes initiate mood swings. They alter hormonal balances. This can affect emotional regulation.
- Pain Relievers: Opioid painkillers are another area of concern. Chronic use can lead to depression. Their potential for addiction adds another layer of complexity.
- Anti-Anxiety Medications: Paradoxically, some anti-anxiety drugs can worsen depressive symptoms. This highlights the importance of accurate diagnosis.
- Antibiotics: Certain antibiotics can influence gut bacteria. The gut microbiome has a crucial role concerning mental health. This relationship deserves more research.
Recognizing the Signs: Spotting Drug-Induced Depression
Recognizing the symptoms is the initial step. It is not always easy to identify the cause. The symptoms may resemble other forms of depression. You should remain vigilant about potential side effects. Common indicators include:
- Persistent sadness or emptiness.
- Loss of interest in activities.
- Changes in appetite or sleep patterns.
- Feelings of hopelessness.
- Difficulty concentrating.
- Thoughts of self-harm or suicide.
If you experience any of these, assess your medications. Also, consult a healthcare professional.
A Call to Action: Taking Control of Your Mental Health
You are not powerless. There are steps you can take. They can help manage drug-induced depression.
- Open Communication: Talk to your doctor. Disclose all medications. Discuss any concerning symptoms.
- Medication Review: Your doctor may adjust dosages. They might switch medications. Don't make changes on your own.
- Seek Therapy: Therapy is often incredibly beneficial. Cognitive Behavioral Therapy (CBT) is effective. It can help manage negative thoughts.
- Lifestyle Adjustments: Focus on overall wellness. Regular exercise and a healthy diet can significantly help your mood. Get adequate sleep. Limit alcohol consumption.
- Support Network: Build a strong support system. Talk to loved ones. Joining a support group can also be valuable.
The Importance of Openness: Fostering a Dialogue
We should eliminate the stigma surrounding mental health. It is critical to create an open dialogue. This helps people seek help without shame. It also encourages people to voice their concerns. Discuss your medication with doctors. Ensure you understand the possible risks. Don't hesitate to ask for help if you are struggling.
A Final Thought: Prioritizing Holistic Well-being
Drug-induced depression is a serious issue. It can have a significant impact on people's lives. Always remember that you are not alone. Openness and education are paramount. Taking proactive steps will help you live a healthier, more fulfilling life. Prioritize your mental wellness. It is just as vital as your physical health.
Is That PMS or Depression? The Shocking Truth About Premenstrual DepressionDrug-Induced Depression: Shocking Truth You Need to Know!
Hey there, fellow health enthusiasts! Ever felt like you were caught in a relentless downpour of gloom, even when the sun should be shining? Maybe you're not alone. We're going to dive deep into something that often flies under the radar: drug-induced depression. It's a sneaky condition, a silent saboteur, and understanding it is crucial for taking back control of your mental well-being. We’re going to explore the nitty-gritty, the shocking truths, and what you can do about it. Buckle up, because this is important stuff!
1. The Unexpected Hangover: What is Drug-Induced Depression?
Think of it like this: you’re on a fantastic vacation, enjoying the scenery, the food, the company. Suddenly, a rogue wave crashes over you, dragging you down. That rogue wave, in this case, is a medication that's causing the emotional equivalent of a hurricane. Drug-induced depression (DID) is essentially depression triggered as a side effect of a medication you're taking. This isn't about feeling a bit blue after a tough day; we're talking about a sustained period of low mood, hopelessness, loss of interest in activities, and often, a whole host of other symptoms. It's a real medical condition, and it's more common than you might think. We'll unravel the threads, one by one.
2. The Culprits Revealed: Common Medications That Can Trigger D.I.D.
Okay, let's get real. This isn't about demonizing medication; it’s about awareness. Many medications, lifesaving or aiding various conditions, can unfortunately have the side effect of impacting our mental health. Think of them as double-edged swords. Some common culprits include:
- Corticosteroids (like prednisone): Used for a variety of inflammatory conditions, from asthma to arthritis.
- Beta-blockers: Often prescribed for high blood pressure and heart conditions.
- Certain Antibiotics: Particularly those that impact the gut microbiome, the importance of which we'll discuss shortly.
- Hormonal contraceptives: Yes, birth control pills can potentially affect mood.
- Some medications for Parkinson's disease and seizures.
- Statins: Used to lower cholesterol.
This isn't an exhaustive list, and the effects can vary wildly from person to person. The key takeaway? Always check with your doctor or pharmacist about potential side effects, and never hesitate to voice your concerns.
3. Hidden Undercurrents: How Do Drugs Actually Cause Depression?
This is where things get fascinating—and a little scientific! The exact mechanisms aren’t always fully understood, but several factors play a role. Drugs can impact:
- Neurotransmitters: The chemical messengers in your brain. Many medications interfere with the delicate balance of serotonin, dopamine, and norepinephrine – the "feel-good" chemicals. Think of it as messing with the sound system in the concert hall of your mind.
- Brain Inflammation: Some medications can trigger inflammation in the brain, which is increasingly linked to depression.
- Gut-Brain Axis: This is a hot topic in modern medicine. Your gut health has a profound impact on your mental health. Some drugs disrupt the balance of your gut microbiome, potentially contributing to mood disorders.
4. Spotting the Signs: Recognizing the Symptoms of D.I.D.
Knowing the symptoms is like having a map in a dense forest. The symptoms of drug-induced depression are very similar to those of "regular" depression. They can include:
- Persistent sadness, emptiness, or hopelessness.
- Loss of interest or pleasure in activities you used to enjoy.
- Changes in appetite or weight.
- Sleep disturbances (insomnia or sleeping too much).
- Fatigue or loss of energy.
- Feelings of worthlessness or guilt.
- Difficulty concentrating, remembering, or making decisions.
- Thoughts of death or suicide.
The crucial clue is the temporal association between starting a medication and the onset of these symptoms. Did your mood plummet shortly after you began taking a specific drug? That's a major red flag.
5. The "Why Me?" Factor: Who's at Higher Risk?
Some people are simply more vulnerable. Factors that can increase your risk include:
- Pre-existing mental health conditions: If you've experienced depression or anxiety before, you're already playing on a field that's prone to emotional storms.
- Family history of depression: Genes absolutely play a role.
- Certain medical conditions: Chronic illnesses, and conditions affecting hormone levels.
- Age and demographics: Research indicates certain age groups are more susceptible.
- Polypharmacy: Taking multiple medications simultaneously increases your risk.
- Individual Biology: How the human body reacts to the introduced substances.
6. The Crucial Conversation: Talking to Your Doctor
This is absolutely vital. If you suspect a medication is affecting your mood, talk to your doctor. Don't suffer in silence! Be open, honest, and specific about your symptoms. Your doctor can:
- Evaluate your symptoms and rule out other causes.
- Assess and possibly adjust your medications (e.g., lowering the dose, changing to a different drug, or adding an antidepressant).
- Recommend therapy and/or lifestyle changes.
- Refer you to a mental health professional.
7. Weighing the Options: Managing Drug-Induced Depression
There might be no 'one size fits all' solution here. Managing DID often involves a multi-pronged approach:
- Medication adjustments: The most direct approach may be to re-evaluate the medication.
- Therapy: Talk therapy, particularly Cognitive Behavioral Therapy (CBT), can be incredibly helpful.
- Lifestyle changes: Exercise, a healthy diet, enough sleep, and stress-reduction techniques are critical.
- Support system: Lean on your friends, family, and/or support groups.
8. The Power of Patience: Time and Recovery
Recovery from DID isn't always instantaneous. It takes time, patience, and the right support. Be kind to yourself. There will be ups and downs, but with the right approach, you can regain your emotional equilibrium.
9. The Role of Diet and Nutrition: Fueling Your Brain
What you eat matters, big time. Some research indicates that:
- Omega-3 Fatty Acids: Found in fatty fish (salmon, tuna) and flaxseeds, have been linked to improved mood.
- Probiotics: Support a healthy gut microbiome, possibly aiding mental health.
- Antioxidant-rich foods: Fruits and vegetables can help mitigate oxidative stress.
- Foods to avoid: Processed foods, sugary drinks, and excessive alcohol.
10. The Exercise Prescription: Moving Your Way to Better Mood
Exercise is a potent antidepressant. It releases endorphins, reduces stress, and improves sleep. Find an activity you enjoy – walking, dancing, swimming, anything that gets your body moving!
11. Mindfulness and Meditation: Cultivating Inner Peace
These practices can help calm your mind, reduce stress, and increase your self-awareness. Even a few minutes of daily meditation can make a difference.
12. Building a Support Network: You're Not Alone
Reach out to friends, family, or a mental health support group. Sharing your experiences and connecting with others who understand can be incredibly empowering.
13. The Importance of Sleep: Restoring Your Mind
Sleep deprivation is a major mood killer. Aim for 7-9 hours of quality sleep each night. Establish a regular sleep schedule, create a relaxing bedtime routine, and avoid caffeine and alcohol before bed.
14. Alternative Approaches: Exploring Additional Opportunities
While not a replacement for standard medical care, some complementary therapies, such as:
- Acupuncture.
- Aromatherapy.
- Herbal supplements (discuss with your doctor first!).
May provide additional support.
15. The Future of Mental Health: Where Are We Headed?
Research is constantly evolving. We can hope for:
- More personalized medicine.
- Better understanding of the brain-gut connection.
- More effective and targeted treatments.
The more we learn, the better equipped we will be to combat drug-induced depression at its root.
Closing Thoughts:
Dealing with drug-induced depression can feel like navigating a labyrinth, but let me be clear: there is hope. By understanding the causes, recognizing the symptoms, and taking proactive steps, you can reclaim your emotional well-being. Remember, you're not alone in this journey. Seek support, be patient with yourself, and celebrate every small victory. You got this!
FAQs (Frequently Asked Questions):
1. Can drug-induced depression be cured?
While there isn't a "cure" in the traditional sense, drug-induced depression is often reversible. By identifying and addressing the underlying cause (the medication), and implementing treatment strategies (therapy, lifestyle changes, potentially antidepressant drugs), you can experience significant improvement and a return to your baseline.
2. How quickly does drug-induced depression go away after stopping the medication?
It varies greatly depending on the individual, the medication, and the severity of the depression. It can take anywhere from a few weeks to several months.
Escape the Darkness: One Baker's Secret Weapon Against DepressionHow do antidepressants work - Neil R. Jeyasingam

By TED-Ed How do antidepressants work - Neil R. Jeyasingam by TED-Ed
The Relationship Between Depression & Drug Misuse mentalhealth drugaddition

By The Recovery Village Drug and Alcohol Rehab The Relationship Between Depression & Drug Misuse mentalhealth drugaddition by The Recovery Village Drug and Alcohol Rehab
Life-Changing Drug Fights Depression in Hours

By ABC News Life-Changing Drug Fights Depression in Hours by ABC News

Title: Tablets for depression - Do antidepressants help DW Documentary
Channel: DW Documentary
Tablets for depression - Do antidepressants help DW Documentary by DW Documentary
Is YOUR Child Secretly Depressed? This Tool Reveals the TRUTH!
Drug-Induced Depression: Shocking Truths That Demand Your Attention!
We live in a world saturated with pharmaceuticals. The promise of relief, of a return to normalcy, is a powerful motivator, and understandably so. However, nestled within this landscape of hope lies a less-discussed reality: the potential for certain medications to induce, or significantly worsen, the very condition they are often prescribed to alleviate. This article delves into the often-overlooked connection between pharmaceuticals and the insidious onset of depression, offering a critical examination of the drugs implicated, the mechanisms involved, and, crucially, what you need to know to protect your mental well-being.
The Pharmacological Tightrope: When Medication Works Against You
The human brain is a complex tapestry of neurotransmitters, receptors, and intricate pathways. Medications, designed to interact with these systems, can have profound effects, both positive and negative. While many drugs offer life-altering benefits, it's essential to acknowledge that some, in their interaction with the brain's delicate balance, can trigger depressive episodes. The reasons why this occurs are multifaceted, ranging from direct disruptions of neurotransmitter function to broader systemic effects. For instance, certain medications can deplete or interfere with the production of serotonin, dopamine, and norepinephrine – the very neurotransmitters crucial for mood regulation, motivation, and feelings of pleasure.
Common Culprits: A Closer Look at Depression-Inducing Medications
Identifying the specific medications most frequently associated with drug-induced depression is paramount. While the effects can vary from individual to individual, the following categories of drugs have consistently demonstrated a link to depressive symptoms:
- Beta-Blockers: Commonly prescribed for cardiovascular conditions like high blood pressure and angina, beta-blockers work by slowing the heart rate and reducing blood pressure. However, these drugs can also cross the blood-brain barrier, affecting neurotransmitter activity. Propranolol, in particular, has been linked to instances of clinical depression.
- Corticosteroids: These powerful anti-inflammatory drugs, such as prednisone, are frequently used to treat conditions like arthritis, asthma, and inflammatory bowel disease. Long-term use or high doses of corticosteroids can disrupt the hypothalamic-pituitary-adrenal (HPA) axis, a crucial system involved in stress response and mood regulation.
- Hormonal Medications: The hormonal landscape can be significantly altered by medications, including oral contraceptives. Some women experience mood changes, including depressive symptoms, while taking birth control pills containing synthetic hormones. Additionally, hormone replacement therapy (HRT) requires careful monitoring for potential psychiatric side effects.
- Statins: Prescribed to lower cholesterol levels, statins have been the subject of ongoing debate regarding their potential impact on mood. Some studies have suggested a link between statin use and increased risk of depression, although the evidence remains inconclusive.
- Anticonvulsants: Certain medications used to treat seizures and bipolar disorder, such as topiramate and levetiracetam, have been associated with an increased risk of depression and suicidal ideation.
- Opioid Pain Relievers: The long-term use of opioid painkillers, while offering relief from chronic pain, can lead to a host of complications, including depression. The mechanisms behind this association are complex, possibly involving alterations in neurotransmitter systems.
- Certain Antibiotics: While less common, some antibiotics, particularly those affecting the gut microbiome, may indirectly influence mood. The gut-brain axis, a complex communication pathway between the gut and the brain, plays a critical role in mental health.
Unraveling the Mechanisms: How Drugs Trigger Depression
Understanding the ways in which these medications induce depression is essential for effective prevention, diagnosis, and treatment. Several distinct mechanisms are at play:
- Neurotransmitter Depletion: Many drugs work by interfering with the production, release, or reuptake of essential neurotransmitters like serotonin, norepinephrine, and dopamine. For example, some beta-blockers impair the production of serotonin. Low levels of these neurotransmitters are strongly correlated with depressive symptoms.
- HPA Axis Disruption: The HPA axis is the body's primary stress response system. Corticosteroids can suppress the normal function of this axis leading to an imbalance of cortisol, a stress hormone, and other key components resulting in depression.
- Inflammation: Some medications may trigger or exacerbate inflammation in the brain. Chronic inflammation is increasingly recognized as a contributing factor to the development of depression.
- Gut Microbiome Alterations: Certain antibiotics and other medications can disrupt the delicate balance of bacteria in the gut. This alteration can affect the gut-brain axis and, consequently, mood regulation.
- Direct Brain Receptor Effects: Some drugs bind directly to receptors in the brain, altering the sensitivity and activity of these receptors. This can disrupt normal brain function and increase the risk of depression.
- Drug Interactions: Taking multiple medications concurrently can increase the risk of adverse side effects, including depression. Drug interactions can occur when two or more medications interfere with each other, resulting in an unexpected outcome like an increase in depressive symptoms.
Recognizing the Signs: Identifying Drug-Induced Depression
Prompt recognition of drug-induced depression is crucial for minimizing its impact. The symptoms can mirror those of other forms of depression, but there are often subtle clues pointing to a medication-related cause:
- Onset Timing: The development of depressive symptoms shortly after starting a new medication or increasing the dosage of an existing one is a significant red flag.
- Unexplained Symptoms: The absence of a clear underlying cause, such as a traumatic event or significant life stressor, should raise suspicion.
- Correlation with Dosage: Symptoms may worsen with increasing medication dosages.
- Resolution After Medication Change: Symptoms often improve or resolve after the offending medication is discontinued or the dosage is adjusted.
What You Can Do: Proactive Steps to Protect Your Mental Health
You are not powerless in the face of potential drug-induced depression. Proactive steps can significantly reduce your risk and help you maintain your mental well-being:
- Open Communication: Talk openly to your doctor about your medications. Discuss any concerns you have about potential side effects, including mood changes.
- Detailed Medication List: Keep an updated list of all medications you are taking, including over-the-counter drugs, supplements, and herbal remedies. Sharing this with your doctor ensures proper monitoring.
- Regular Monitoring: If you are taking a medication known to be associated with depression, schedule regular check-ups with your doctor to monitor your mood and any signs of adverse effects.
- Second Opinions: Seek a second opinion from another doctor or psychiatrist if you have concerns about a medication or if you’re experiencing persistent depressive symptoms.
- Mind-Body Practices: Engage in regular exercise, mindfulness meditation, and yoga. These practices have been shown to reduce stress, improve mood, and promote overall mental well-being.
- Healthy Diet: Consume a nutrient-rich diet focused on whole foods, including fruits, vegetables, and lean proteins. Avoid excessive consumption of processed foods, sugar, and alcohol.
- Prioritize Sleep: Aim for 7-9 hours of quality sleep each night. Disrupted sleep patterns are linked to depression.
- Therapy and Support: Consider therapy or counseling, particularly cognitive-behavioral therapy (CBT), a proven effective treatment for depression. Build and maintain a strong support network of friends and family.
Taking Control of Your Well-Being
Drug-induced depression is a complex issue, but by arming yourself with knowledge and taking proactive steps, you can significantly reduce your risk and protect your mental health. Open communication with your healthcare providers, careful medication management, and a commitment to a healthy lifestyle are essential. Remember, you are the ultimate advocate for your own well-being. By staying informed and engaged, you can navigate the world of medication with greater confidence and maintain a fulfilling, mentally healthy life.
