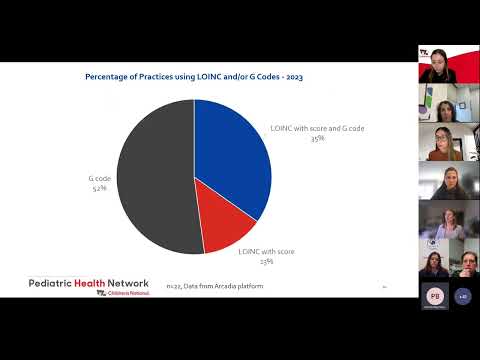
Title: PHN Quality Improvement Initiative Depression Screening & Follow up Project Kick Off
Channel: Pediatric Health Network
PHN Quality Improvement Initiative Depression Screening & Follow up Project Kick Off by Pediatric Health Network
depression screening follow up, depression screening and follow up for adolescents and adults, depression screening and follow up ecqm, postpartum depression screening and follow up, prenatal depression screening and follow up, uds depression screening and follow up, phq 9 depression screening and follow up plan, depression screening results, depression screening symptoms, depression follow up guidelines
Depression Screening Follow-Up: Did Your Results SHOCK You?
Navigating the Aftermath: What Happens After Your Depression Screening?
It's a brave step, taking that initial plunge into mental health screening. You did it! You faced the questionnaire. Perhaps the results buzzed with an unexpected revelation. Now what? That feeling, a mixture of curiosity and anxiety, is completely normal. Let's unpack the post-screening journey, shall we?
Understanding Your Score: Beyond the Binary
The numbers are in. But what do they really mean? Firstly, resist the urge to self-diagnose. Screening tools provide a valuable snapshot, not a definitive verdict. The score gives a clue, a starting point. Consider it a flag, not a sentence.
Also, understand that these screeners aren't perfect. They are tools. The information should guide, not define. Various factors influence your score. Things like current life stressors, recent events, and even physical health play a role.
Decoding the Next Steps: A Roadmap Ahead
So, your screening yielded some intriguing data. What’s next? The follow-up. This will typically involve a conversation with a healthcare professional. This person will be a doctor, therapist, or counselor.
The conversation is crucial. They will dive deeper. Expect probing questions about your mood, sleep patterns, and energy levels. Anticipate sharing your experiences in detail. Expect your provider to listen attentively. They want to understand you, as a whole person.
The Power of Professional Insight: Unveiling Hidden Dimensions
The healthcare professional's skill set shines in this setting. They provide clarity. They are trained to interpret complexities. They can differentiate between transient feelings and persistent symptoms.
Additionally, they can help you access tailored support. This help may include therapy, medication, or lifestyle modifications. The goal is always to offer the best path for your journey. This is unique to you.
Therapy: Your Partner in Progress
Therapy is a key component of many treatment plans. It creates a safe space. Here, you can explore your feelings. You can learn coping mechanisms. You can process your experiences.
There are different types of therapy. Cognitive Behavioral Therapy (CBT) targets negative thought patterns. Interpersonal Therapy (IPT) focuses on relationships. Dialectical Behavior Therapy (DBT) helps manage intense emotions.
So, explore your options. Find a method that resonates with you. The therapist guides your process. It is a partnership.
Medication: A Supportive Tool
For some, medication offers significant relief. Antidepressants can balance brain chemicals. They won't magically fix things. They can improve your mood. They may help with sleep or appetite.
However, medication is not a quick fix. It often takes time to find the right medication and dosage. Stay patient. Work closely with your doctor. Regularly discuss side effects and changes.
Lifestyle Boosters: Small Changes, Big Impact
Beyond professional treatment, lifestyle adjustments can make a big difference. Exercise boosts mood. Eating a balanced diet supports your body. Prioritizing sleep improves mental clarity.
Also, connect with others. Social support is vital. Join a support group. Talk to friends or family. These small acts make a huge impact.
Monitoring Your Progress: Staying the Course
Recovery is a process, not an event. It's essential to monitor your progress. Regularly check in with your healthcare provider. Communicate how you're feeling. Track improvements and challenges.
Therefore, don't hesitate to adjust your treatment plan. What works today might not work tomorrow. Be flexible. Be proactive.
Embracing Resilience: The Path Forward
The journey of addressing mental health requires courage. It asks for vulnerability. Recognize your strength in taking the screening. Celebrate your willingness to seek help.
Remember, you are not alone. Many people experience depression. Effective treatments are available. It is possible to feel better.
So, be kind toward yourself. Practice self-compassion. Celebrate small victories. Every step you take toward recovery is a triumph. You've got this! And always, seek expert guidance.
Depression Glass: The SECRET Marks Only Experts Know!Depression Screening Follow-Up: Did Your Results SHOCK You?
Hey everyone, let’s get real for a minute. Mental health… it’s a journey, not a destination. And sometimes, that journey takes us down roads we never expected. We're diving deep today into something intensely personal, yet incredibly common: the follow-up to a depression screening. Did your results shock you? Maybe you thought you were doing okay, or maybe you knew something was brewing beneath the surface. Whatever the case, we're here to unpack the feelings, the questions, and the next steps. Because, trust me, you're not alone. We'll be navigating the emotional landscape, offering support, and remembering that seeking help is a sign of strength, not weakness.
1. The Initial Screening: That Moment of Truth
Think back to that initial screening. Maybe it was a routine check-up, a moment of quiet reflection in an online questionnaire, or a chat with your doctor. Either way, it was the first step. It was like a mirror reflecting back a picture of your emotional well-being. For some, it might have been a casual glance, like seeing a slightly crooked smile. For others, it might have felt like staring into a funhouse mirror, distorting and revealing truths they weren’t quite prepared for. That initial score… was it higher than you anticipated? Did it confirm a nagging feeling, or did it blindside you entirely?
2. Decoding the Screening Tools: It's Not Rocket Science (But it's Important)
Let's demystify the actual tools used. These aren’t magic wands; they're questionnaires, checklists, and sometimes, conversations that help gauge your mood, sleep patterns, appetite, and overall interest in life. The most common tools include the PHQ-9 (Patient Health Questionnaire-9), GAD-7 (Generalized Anxiety Disorder 7-item scale), and others. They often ask about things like feeling down, experiencing changes in sleep or appetite, or having thoughts of harming yourself. Knowing what questions are being asked and the kinds of symptoms they address can help you to understand the potential outcomes.
3. The Emotional Rollercoaster: Processing the Results
Once you have those results, the real work begins: processing them. This can be tough. It’s like a raw wound suddenly exposed. You might feel a whirlwind of emotions: shock, denial, shame, relief, or a confusing mix of everything. Don’t worry, feeling overwhelmed is normal. Give yourself permission to feel what you feel. This isn't a race; it's a marathon. Allow yourself the time and space to absorb the information. Think of it like a puzzle – you've got the pieces, now you have to figure out how they fit together.
4. Shock, Surprise, and the “I Didn't Know I Was That Depressed” Moment
This one’s a biggie. Often, the most challenging part of the screening is the "I didn't know" feeling. It's like realizing that a tiny leak in the roof has quietly been causing a flood. Depression can creep in, slowly eroding your joy, motivation, and sense of self without you even realizing the full extent of its impact. You might be surprised to discover the severity of your condition. The screening may highlight symptoms you'd dismissed as "just having a bad day" or "feeling a bit down." It’s okay to feel surprised, even a bit embarrassed. But remember, acknowledging the problem is the first giant step towards healing.
5. Understanding the Different Faces of Depression: A Quick Glance
Depression isn't one-size-fits-all. It comes in many forms:
- Major Depressive Disorder: The classic “clinical depression,” marked by persistent sadness, loss of interest, and physical symptoms.
- Persistent Depressive Disorder (Dysthymia): A milder but more chronic form, often characterized by a low-grade, persistent sadness.
- Seasonal Affective Disorder (SAD): Depression linked to changes in seasons, typically starting in fall and lasting through winter.
- Postpartum Depression: Depression related to childbirth.
- Bipolar Disorder: While primarily a mood disorder, depressive episodes are a key feature.
- Situational depression: Temporary depression triggered by a life event, usually short-lived.
Recognizing the type of depression you're experiencing can help in finding the right treatment.
6. The Follow-Up Appointment: What to Expect
So, you've gotten your results, and now you have a follow-up appointment. What happens? This is your chance to discuss your results in detail with a healthcare professional. Be prepared to talk openly and honestly about your symptoms, your history, and your experiences.
- Detailed Discussion: The doctor will likely ask in-depth questions about the symptoms identified during the screening tool.
- Further Assessment: They may perform another evaluation, which will take into account your mental state and medical history to confirm the diagnosis and decide on treatment.
- Treatment Options: Your doctor or therapist will discuss treatment options, which is the critical step.
7. Breaking Down the Stigma: You Are Not Alone
Let's smash the stigma surrounding mental health! Seriously, it's a huge problem. Too often, people are ashamed to acknowledge they're struggling, which prevents them from getting help. Depression is a medical condition, just like diabetes or a broken arm. It's not a moral failing, or a sign of weakness. It is a sign of being human. Mental health is extremely crucial. Speak up, and seek help. Remember, countless others have been where you are now.
8. The Power of Sharing: Talking to Loved Ones
This one can be tricky, but it's often essential. Sharing your results with trusted friends and family can provide invaluable support, but consider it one step at a time. Choose people you feel comfortable with, people who will listen without judgment. It's okay if they don't fully understand; their support and empathy matter more than their expertise. Communicating with your network can strengthen your support system and help reduce feelings of isolation.
9. Therapy: The Cornerstone of Healing
Therapy is often the cornerstone of depression treatment. Whether it's individual, group, or family therapy, it provides a safe space to explore your feelings, learn coping mechanisms, and develop strategies for managing your symptoms.
- Cognitive Behavioral Therapy (CBT): Helps you identify and change negative thought patterns and behaviors.
- Psychodynamic Therapy: Explores past experiences and how they affect your present feelings.
- Interpersonal Therapy (IPT): Focuses on improving your relationships and communication skills.
Finding the right therapist is key. It’s about finding a person you can trust, and who feels like a good fit for your personality.
10. Medication: When It’s Necessary
Medication can be an important part of treatment for some people. Antidepressants work by balancing the chemicals in your brain that affect your mood. It's essential to work closely with your doctor when taking medication. They can help you find the right medication, monitor side effects, and adjust dosages as needed. Never stop or change the dosage of your medication without consulting your doctor.
11. Lifestyle Changes: The Everyday Allies
Beyond therapy and medication, lifestyle changes can play a massive role in managing depression.
- Exercise: Physical activity releases endorphins, which have mood-boosting effects.
- Healthy Diet: Nourishing your body with nutritious foods can improve your overall well-being.
- Sleep Hygiene: Establishing a regular sleep schedule can improve your mood and energy levels.
- Mindfulness and Meditation: These practices can help you manage stress and anxiety.
Tiny changes can create significant benefits.
12. Finding Your Support System: Builders of Positivity
Your support system is your army. This can include your family, friends, therapist, support groups, or even online communities. Surround yourself with people who uplift you, encourage you, and understand what you’re going through. Let them know how they can best support you. Support groups can be especially helpful, as they connect you with people who understand the realities of depression.
13. Setting Realistic Expectations: It's a Process, Not a Quick Fix
Healing from depression is not a miraculous journey. It’s a process. It takes time, effort, and patience. There will be ups and downs. Some days will be tougher than others. Celebrate the small victories. Acknowledge your progress, even when it feels slow. Be kind to yourself. Remember that you are stronger than you realize.
14. The Role of Self-Care: Nurturing Your Inner Self
Self-care isn't selfish; it's essential. It’s about making time for activities that bring you joy, reduce stress, and nourish your mind, body, and soul. This could include anything from taking a relaxing bath to reading a book, spending time in nature, or pursuing a hobby. Make self-care a consistent part of your routine, like your daily dose of medicine.
15. Building a Sustainable Recovery: The Goal
The ultimate goal is a sustainable recovery. This means not just managing your symptoms but building a life filled with meaning, purpose, and joy. It involves developing coping skills, strengthening your support system, and learning to live with any lingering challenges. Recovery is the journey, not just the destination. It's about finding your equilibrium, and living a life that feels
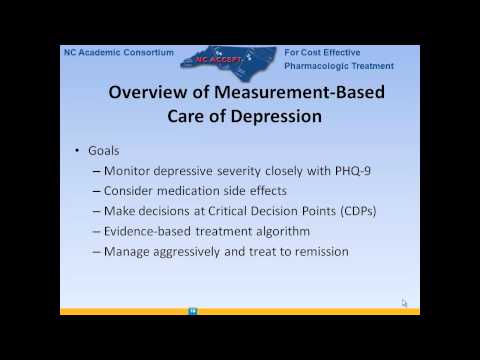
Escape the Darkness: Shocking New Depression Medicine Uses Revealed!Treating Depression in the Primary Care Setting with Dr. Sager

By UofL Internal Medicine Lecture Series Treating Depression in the Primary Care Setting with Dr. Sager by UofL Internal Medicine Lecture Series
IPRO ESRD Defining the Six Conditions of the Depression Screening in EQRS

By IPRO ESRD Network Program Channel IPRO ESRD Defining the Six Conditions of the Depression Screening in EQRS by IPRO ESRD Network Program Channel
Major Depressive Disorder Leveraging the PCMH Model to Improve Patient-Centered Management

By HMP Education Major Depressive Disorder Leveraging the PCMH Model to Improve Patient-Centered Management by HMP Education
Title: Internal Medicine Grand Rounds - Managing Depression in Primary Care
Channel: ECUIM
Internal Medicine Grand Rounds - Managing Depression in Primary Care by ECUIM
Is This the Silent Killer? The Shocking Truth About the Depression & Anxiety Epidemic
Depression Screening Follow-Up: Did Your Results Shock You?
We live in a world increasingly attuned to mental well-being. Conversations once relegated to hushed corners are now blossoming into open dialogues, with mental health resources readily accessible. One crucial tool in this evolving landscape is the depression screening. If you've recently undergone such a screening, the results may have been surprising, even unsettling. This article will delve into the crucial next steps following a depression screening, empowering you with the knowledge and support you need to navigate this potentially challenging period.
Understanding the Initial Screening: Beyond the Surface-Level Questions
The depression screening itself is a carefully constructed process. These screenings, often administered via questionnaires, are not intended to diagnose but rather to identify the potential presence of depressive symptoms. The questions – probing your mood, sleep patterns, appetite, and energy levels – are designed to detect patterns that may indicate a need for further evaluation. These initial screenings typically use validated scales like the Patient Health Questionnaire-9 (PHQ-9) or the Generalized Anxiety Disorder 7-item scale (GAD-7)
The numerical scores from these assessments represent a preliminary gauge. They are not meant to be definitive pronouncements. Instead, they are valuable indicators, serving as the starting point for a more comprehensive evaluation. The screening’s simplicity belies its significant power: to prompt self-reflection and initiate a conversation about your mental health.
Decoding Your Scores: What the Numbers Really Mean
The interpretation of your screening results should be made by a qualified professional. The results are typically categorized into ranges, with each range reflecting a different level of potential concern. For example, a PHQ-9 score of 0-4 might indicate minimal or no symptoms, while a score of 10-14 might suggest moderate depression. However, the precise interpretation varies depending on the specific screening tool used and the individual's specific circumstances.
It is critical to understand that these scores are not etched in stone. They represent a snapshot in time. Your mental state can fluctuate, and a single screening cannot capture the full complexity of your emotional experience. Your healthcare provider will use these scores, alongside a detailed discussion, to formulate a complete understanding of your mental state. Open and honest communication is paramount.
The Critical Follow-Up: Actionable Steps After Your Screening
The screening process is only the beginning. The follow-up is where the real work begins. If your screening suggests potential concerns, your healthcare provider will likely recommend a follow-up appointment. This follow-up is not merely a formality; it is a vital opportunity to delve deeper into your experiences and initiate any necessary interventions.
During this follow-up, you'll have the opportunity to share more details about your symptoms, including their duration, intensity, and impact on your daily life. The healthcare provider will likely ask you questions about your personal history, family history of mental illness, and any current stressors in your life. They will also ask if any triggers, such as trauma, loss, or other emotional events, have impacted your mental well-being.
Exploring Diagnostic Possibilities: Beyond the Simple Screening
Based on your screening results and follow-up discussion, your healthcare provider may recommend a formal diagnosis. It is essential to understand the distinction between the screening and a diagnosis. A screening is a preliminary assessment, while a diagnosis involves a more comprehensive evaluation, often by a psychiatrist or psychologist.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides criteria for diagnosing various mental health conditions, including depression. A formal diagnosis typically involves a detailed assessment of your symptoms, their duration, and their impact on your functioning. Additional considerations are any past medical history, including traumatic events such as abuse, serious accidents, the death of someone close to you, and other significant emotional burdens.
Treatment Options: A Personalized Approach to Recovery
Treatment for depression is highly individualized. The best treatment plan for you will depend on various factors, including the severity of your symptoms, the underlying causes of your depression, and your personal preferences. Several treatment modalities are available, and often a combination of approaches is most effective.
1. Psychotherapy: Finding Your Voice and Healing
Psychotherapy, often referred to as "talk therapy," is a cornerstone of depression treatment. Different therapeutic approaches are used, including cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and interpersonal therapy (IPT). CBT focuses on identifying and changing negative thought patterns and behaviors. DBT emphasizes emotional regulation and distress tolerance, and IPT addresses difficulties in relationships and social functioning.
2. Medication: An Important Tool, Not a Universal Solution
Antidepressant medications can be a valuable tool for managing depressive symptoms. These medications work by influencing the levels of neurotransmitters, such as serotonin and norepinephrine, in the brain. Finding the right medication and dosage may require some trial and error, so it is essential to work closely with your healthcare provider and report any side effects.
3. Lifestyle Modifications: Supporting Your Mental Well-being
Alongside therapy and medication, lifestyle modifications can significantly impact your mood. Regular exercise, a balanced diet, sufficient sleep, and stress-management techniques are all vital components of a holistic approach to recovery. Mindful practices, such as meditation and yoga, can also be powerfully helpful in reducing stress and improving mood.
4. Support Systems: Building Your Circle of Resilience
Having a strong support system is crucial for navigating the challenges of depression. This might include family members, friends, support groups, or mental health professionals. Sharing your experiences with others who understand what you're going through can reduce feelings of isolation and promote a sense of connection.
Coping with Disappointment and Uncertainty
Sometimes, screening results, particularly if they suggest a potential mental health concern, can be disheartening. You might experience a range of emotions, from denial to fear. It's crucial to acknowledge these feelings without judgment. Allow yourself space to process your emotions, and remember that seeking help is a sign of strength, not weakness.
It's also essential to embrace the uncertainty that often accompanies mental health challenges. The path to recovery is rarely linear. There may be setbacks along the way. Celebrate small victories, and remember that progress, not perfection, is the ultimate goal.
Advocating for Yourself: Empowering Your Mental Well-being
You are your most important advocate. Take an active role in your treatment. Ask questions, voice your concerns, and express your preferences. Do not hesitate to seek a second opinion if you feel a treatment plan isn't working for you. Research your options and familiarize yourself with the resources available in your community.
Long-Term Wellness: Cultivating a Life of Flourishing
Recovering from depression is not simply about alleviating symptoms; it's about building a life of meaning and flourishing. This involves nurturing your relationships, pursuing your passions, and cultivating a sense of purpose. Prioritize your mental well-being as you would any other aspect of your health. Engage in regular self-care practices, and seek support when needed.
The journey ahead may have its share of challenges, but armed with knowledge, support, and a commitment to your well-being, you can find your path to lasting wellness. Embrace the process, celebrate your progress, and remember that you are not alone.
