
Title: Depression Explained Major Depressive Disorder
Channel: Rhesus Medicine
Depression Explained Major Depressive Disorder by Rhesus Medicine
depression diagnosis racgp, depression in icd 10, getting a depression diagnosis, depression diagnosis icd 10
GPs Reveal SHOCKING Depression Diagnosis Secret!
GPs Reveal SHOCKING Depression Diagnosis Secret!
The Silent Battle Unveiled: A Glimpse into Depression's Shadows
The air crackles with unspoken truths. GPs, those gatekeepers of our well-being, often hold keys to hidden realities. Their insights into the human condition are invaluable. They witness the ebb and flow of emotions daily. They are the first point of contact for many seeking solace. Lately, a collective whisper is circulating amongst these trusted professionals. They are sharing secrets about diagnosing depression. These secrets are quite revealing. They are not always what one anticipates.
Beyond the Surface: Unmasking the Complexity within
Depression is not a simple ailment. It is a multifaceted experience. It permeates every facet of a person's life. It impacts thoughts, feelings, and behaviors. Understanding its nuances is therefore critical. GPs have a unique vantage point. They see the subtle shifts. They recognize the early warning signs. However, their diagnostic process is far from straightforward. It’s a dance of observation, conversation, and intuition.
The Art of Listening: Uncovering the Hidden Narrative
A keen ear is a GP's most potent tool. They listen with intent. They absorb the unspoken. They probe the silent spaces between words. It is this close listening that truly unlocks the secrets. Patient stories are not always linear. They are a tapestry woven with threads of joy and sorrow. Moreover, GPs are skilled at navigating this maze. They help patients articulate their struggles. They create a safe space for vulnerability. Therefore, trust is paramount in this process.
More Than Just Checklists: Person-Centred Care
Medical textbooks offer checklists. These checklists help diagnose standard health issues. However, depression demands a more personal approach. GPs understand this implicitly. They move beyond the prescribed diagnostic criteria. They see the individual, not just the symptoms. They recognize the uniqueness of each patient’s journey. They tailor their approach accordingly. As a result, treatment plans are highly customized.
The Power of Observation: Seeing What Others Miss
Body language speaks volumes. GPs are trained to read these nonverbal cues. A slumped posture or averted gaze can tell a story. Changes in grooming habits provide clues. These subtle signals can be instrumental in a diagnosis. They combine these observations with patient reports. Consequently, the diagnosis becomes more accurate. They look for patterns and inconsistencies. They know the signs often go unnoticed.
The Role of Empathy: A Healing Touch
Empathy is the cornerstone of effective care. A GP must put themselves in their patient's shoes. They must understand the emotional weight. They must validate their feelings. This connection can be powerful. It helps patients feel seen and heard. It fosters a sense of hope. It's a crucial component of the healing process. Consequently, it builds an unbreakable bond.
The Unexpected Clues: Beyond the Obvious Signs
Depression expresses itself in diverse ways. It's not always sadness and lethargy. Sometimes it manifests as irritability. Other times, it appears as physical pain. GPs are therefore trained to recognize these atypical presentations. They consider the whole picture, not just the blatant symptoms. They ask the right questions to uncover the truth. Frequently, the underlying cause reveals itself.
The Collaborative Approach: A Network of Support
Diagnosing and treating depression is not a solitary endeavor. GPs often collaborate with other specialists. They may refer patients to therapists or psychiatrists. They may also involve family members. This teamwork enhances the quality of care. It ensures the patient receives comprehensive support. Because of this, it creates a holistic treatment plan.
The Secret Weapon: Building Trust
Trust is the lubricant of the doctor-patient relationship. GPs know its critical importance. They cultivate it through active listening. They build it through genuine care. They understand patients will open up when they feel safe. As a result, this trust unlocks deeper insights. The patient will feel comfortable sharing their struggles.
Navigating the Stigma: Breaking Down Barriers
Depression carries a stigma. Many people feel ashamed to seek help. GPs work to dismantle these barriers. They create a non-judgmental environment. They educate patients about the illness. They advocate for mental health awareness. Ultimately, they help those affected feel less alone. They promote openness and honest communication.
The Ongoing Journey: A Path to Healing
The journey of recovery from depression is not always easy. Furthermore, setbacks can occur. GPs provide ongoing support and guidance. They celebrate small victories along the way. They adapt treatment plans as needed. They are steadfast companions on the path to healing. In conclusion, this dedication is commendable.
Is Your Child Secretly Depressed? Shocking Signs You MUST KnowGPs Reveal SHOCKING Depression Diagnosis Secret!
Hey everyone! It's me, and let's be real, talking about mental health can sometimes feel like wading through a swamp. It's often murky, complicated, and full of hidden things. But, as someone who's weathered a few storms in the emotional sea, I'm here to tell you that understanding depression diagnosis doesn't have to be a Herculean task. In fact, we’re about to dive into some secrets – and not the kind you find whispered in dark alleys, but secrets revealed straight From the very people on the frontline: GPs. And believe me, what they share could change how you understand and experience mental well-being.
1. The Silent Struggle: Why Early Diagnosis Matters So Much
Think of depression like a tide. It starts subtle, a slight ebb in your energy and joy, but can quickly transform into a raging storm. Early diagnosis is like having a weather alert system – it gives you time to prepare and protect yourself. We’re not talking about just feeling a bit "down" here: we're talking the full spectrum of depression, from mild to severe. The earlier a GP can identify warning signs, the sooner support can be offered, and the easier it is to navigate the turbulent patches. It can be the difference between riding out the storm and being capsized by it.
2. The GP’s Toolkit: What They're Actually Looking For
So, what exactly are GPs looking for when you sit down in their office, maybe feeling a little blue, or just plain lost? It's not always about the dramatic symptoms seen on TV. GPs are trained to be detectives, piecing together clues. They use a combination of:
- Detailed Questioning: This is where they delve into your history. Expect questions about your sleep, appetite, energy levels, and concentration.
- Observation: They’re watching your body language, voice tone, and the overall presentation. Are you withdrawing? Less engaged than usual?
- Standardized Questionnaires: Tools like the PHQ-9 (Patient Health Questionnaire-9) help quantify symptoms. They’re not perfect, but they provide a helpful framework.
- Excluding Other Physical Causes: Sometimes, symptoms of depression can be caused by other medical conditions, so blood tests might be needed.
3. Beyond the Usual Suspects: Unmasking Hidden Symptoms
Here's where things get really interesting. Often, depression doesn't present itself in the way we expect. It's not always about sadness. Like a chameleon, it can disguise itself as something else. They might start with these few things:
- Physical Pain: Chronic aches, pains, or digestive issues without any clear physical cause.
- Irritability and Anger: Not just sadness, but a short fuse and a general state of frustration.
- Changes in Eating Habits: Significant weight loss or gain.
- Apathy: Loss of interest in things you used to enjoy.
- Changes in Sleep: Insomnia (trouble sleeping) or hypersomnia (sleeping too much).
- Difficulty Concentrating: Feeling fuzzy-headed or struggling to focus.
4. The Gut Feeling Thing: Trusting Your Instincts (and Your GP!)
Okay, let's be honest. The GP’s not a mind reader. But the best ones know how to listen – REALLY listen. A good GP won't dismiss your concerns, even if they seem vague or unrelated. They'll value your perspective and work with you to build a complete picture. Remember, you're the expert on your own experience. Trusting your gut feeling is essential. If you're feeling "off," don't hesitate to bring it up. And don't be afraid to ask questions - lots of them!
5. The Stigma Struggle: Breaking Down the Barriers to Seeking Help
Here's the elephant in the room: Stigma. It's the invisible barrier that stops so many people from seeking help. We live in a society that often glorifies productivity and strength, making it hard to admit struggles. Depression is not a sign of weakness; it is an illness, plain and simple. If you had a broken leg, you wouldn't hesitate to go to the doctor. Taking care of your mental health deserves the same level of care and attention.
6. The Secret Ingredients: Empathetic Communication and Active Listening
A GP's ability to connect with you and understand your experience is crucial. It’s not just about ticking boxes; it's about building trust and creating a safe space to share your fears and challenges. Imagine it as a collaborative dance, where the GP leads, but you are equally part of the experience. Empathy and active listening are the secret ingredients in that dance.
7. Navigating the Maze: The Diagnostic Process Explained
The diagnostic process is often more nuanced than a quick yes/no answer. It might involve several appointments, assessments, and even referrals to specialists. Be patient with the process. It's not always linear, and there might be bumps along the road.
8. Beyond the Diagnosis: Treatment and Support Options
Once diagnosed, the GP will guide you through your treatment options, which might include:
- Therapy: Cognitive Behavioral Therapy (CBT) or talking therapies.
- Medication: Antidepressants.
- Lifestyle Changes: Exercise, diet, sleep hygiene, and social connection.
- Support Networks: Building connections with organizations and support groups.
The key is realizing that it can be like peeling layers of a very complex onion.
9. The Role of the Patient: Active Participation
You are not a passive observer. As a patient, you play a vital role. Be honest in your reporting. Keep track of your symptoms and share everything. Ask questions. Take control of your treatment. It is an important phase in your life.
10. The Importance of a Strong Doctor-Patient Relationship
A strong connection with your GP is a huge advantage. Trust and good communication can dramatically improve your experience and outcomes. Don’t be afraid to shop around for a GP that you click with. It is okay to make a change if you feel that they aren’t listening.
11. The Hidden Costs of Undiagnosed Depression: Why It Matters
Left untreated, depression can impact every aspect of your life – work, relationships, physical health, and overall well-being. The hidden costs are enormous. It can lead to serious problems and even thoughts of self-harm.
12. New Frontiers: Advancements in Diagnosis and Treatment
The good news is that advancements are being made every day! New diagnostic tools, treatment approaches, and a greater understanding of the brain are constantly emerging.
13. Empowering Yourself: Self-Care and Early Warning Signs
You can’t rely on your GP alone. Developing self-awareness and paying attention to warning signs is equally important. Learn your triggers, practice self-care strategies, and seek help early whenever you need it.
14. Sharing the Truth: Why Openness and Honesty Is Important
The more we openly discuss mental health, the more we chip away at the stigma. Sharing your experiences, listening to others, and being willing to talk about depression, can help normalize the conversation and encourage everyone to seek help.
15. The Future of Mental Healthcare: What's on the Horizon?
Mental health is moving towards personalized healthcare and innovative technology. Research continues to improve the speed and accuracy of diagnosis, paving the way for better treatments and support. We are on the brink of a new era of mental healthcare.
In Conclusion: Your Journey, Your Strength
Okay, so we’ve explored the secrets, and frankly, I think that’s pretty exciting, right? Remember this: The path to understanding and managing depression isn't always easy. It’s a journey, sometimes winding, sometimes steep. But you don't have to walk it alone. You are capable and worthy of feeling better. Your mental health matters. Be open to help, and remember that you have the strength to navigate this. And the GPs? They are partners on this journey.
FAQs
1. What if I don't feel "sad"? Can I still be depressed?
Absolutely! Depression manifests in various ways. You may experience physical symptoms, irritability, or a loss of interest in things. It does not always feel sad.
2. How can I prepare for an appointment with my GP about my mental health?
Make a list of your symptoms, when they started, and how they affect your daily life. Also, write down any questions you have.
3. How long does it take to get diagnosed?
There is no one-size-fits-all answer. It may take multiple appointments and assessments to get an accurate diagnosis.
4. What if I'm not comfortable talking to my GP?
It's okay to shop around for a GP that you trust and feel comfortable with. Your relationship with your doctor is important.
5. What if I’m worried about medication?
Discuss your concerns openly with your GP. Discuss all possible options, including therapy and lifestyle changes.
1) Principal Keywords: Depression Diagnosis GPs Revealed 2) SEO Headline: GPs' Shocking Depression Diagnosis Secrets Revealed! 3) Pathway: DepressionSecrets 4) Meta Summary: Discover the shocking secrets GPs reveal about depression diagnosis! Learn about symptoms, treatment, and how to get the help you need.
Europe's Crushing Depression: Are YOU Next?Top 5 Signs Of High Functioning Depression

By Dr Julie Top 5 Signs Of High Functioning Depression by Dr Julie
Why Depressed People Are Very Logical

By HealthyGamerGG Why Depressed People Are Very Logical by HealthyGamerGG
General Practice Mental Health Workforce Needs - RACGP - August 2020
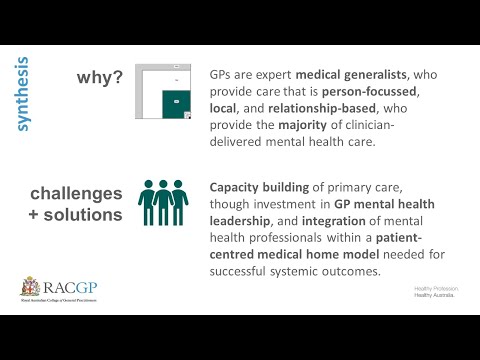
By Michael Tam General Practice Mental Health Workforce Needs - RACGP - August 2020 by Michael Tam

Title: Major Depressive Disorder MDD - Psychiatric Mental Health LevelUpRN
Channel: Level Up RN
Major Depressive Disorder MDD - Psychiatric Mental Health LevelUpRN by Level Up RN
Is Your 11-Year-Old Secretly Depressed? Find Out NOW!
GPs Reveal SHOCKING Depression Diagnosis Secret!
A Silent Epidemic: Unveiling the Hidden Realities of Depression
We, as a society, often grapple with the visible scars of illness. We treat the broken bones, the virulent infections, and the raging fevers with urgency and readily available treatments. Yet, a far more insidious ailment, one that leaves no physical mark but chips away at the very foundations of the self, continues to lurk in the shadows. This is depression, a complex and often misunderstood illness that affects millions worldwide. The shocking truth? The diagnosis and treatment of depression are far more nuanced and challenging than many realize, and recent insights from General Practitioners (GPs) offer a crucial window into these complexities.
The Hidden Indicators: Beyond Sadness and Tears
The stereotypical image of a depressed individual—withdrawn, tearful, and melancholic—is, unfortunately, far too simplistic. While these symptoms can certainly be present, they represent only a fraction of the ways depression manifests. As GPs know all too well, depression is a chameleon, adopting different guises depending on the individual and the specific circumstances of their life.
Consider the following, often overlooked, signs:
- Physical Ailments: Persistent headaches, unexplained aches and pains, digestive issues, and chronic fatigue can all be indicators of an underlying depressive disorder. Patients may visit their GP repeatedly, seeking relief from these physical symptoms, without realizing the root cause lies in their mental state.
- Irritability and Anger: Contrary to the commonly held belief that depression always manifests as quiet sadness, many individuals experience extreme irritability, anger, and frustration. This can lead to interpersonal conflict, strained relationships, and a general sense of being perpetually on edge.
- Changes in Appetite and Sleep: Significant alterations in eating habits and sleep patterns are frequently associated with depression. Some individuals might experience a loss of appetite and struggle to eat, while others may turn to food as a coping mechanism, leading to overeating. Similarly, sleep patterns can be disrupted, with insomnia or excessive sleepiness both being common occurrences.
- Difficulty Concentrating and Making Decisions: Brain fog, forgetfulness, and an inability to focus are pervasive symptoms that can significantly impair an individual's ability to function effectively in daily life. Simple tasks become overwhelming, and decision-making becomes a herculean effort.
- Loss of Interest in Activities: Activities that once brought joy and fulfillment, such as hobbies, social interactions, or even work, begin to lose their appeal. The individual might withdraw from these pursuits, feeling little or no pleasure in what once brought them happiness.
The Diagnostic Maze: Navigating the Challenges of Identification
The initial diagnostic process is rarely straightforward. GPs face the daunting task of sifting through a complex web of symptoms, taking into account the patient's medical history, personal experiences, and lifestyle factors. A diagnosis of depression isn’t simply a matter of ticking boxes on a checklist; it requires a deep understanding of the individual and a careful consideration of the myriad factors that can contribute to the illness.
Key challenges in diagnosis include:
- Comorbidities: Depression often coexists with other conditions, such as anxiety disorders, substance abuse, and chronic pain. These comorbid conditions can obscure the underlying depression, making it more difficult to identify and treat.
- Stigma and Reluctance to Seek Help: The stigma surrounding mental illness remains a significant barrier to diagnosis and treatment. Many individuals, particularly men, are reluctant to admit they are struggling with depression, fearing judgment, shame, or the perception of weakness.
- Limited Time and Resources: GPs are often under immense pressure, with limited time to spend with each patient. This can make it challenging to conduct a thorough assessment and to explore the complexities of a patient's mental health.
- Subjectivity of Symptoms: Unlike physical illnesses that can be objectively measured, the symptoms of depression are often subjective and based on the patient's self-reported experiences. This can make it difficult to accurately assess the severity of the illness and to monitor the effectiveness of treatment.
The Secret Weapon: GPs and the Power of Empathy and Understanding
While these challenges are undeniable, GPs are at the forefront of the battle against depression. They bring to the table not only medical expertise but also crucial skills in communication, empathy, and understanding.
Here’s how they can overcome the hurdles:
- Building Trust: Establishing a strong therapeutic relationship is paramount. GPs often spend years building trust with their patients, creating a safe space for them to disclose their struggles without fear of judgment.
- Active Listening: Taking the time to truly listen to the patient's experiences, without interrupting or dismissing their concerns, is crucial for uncovering the underlying causes of depression.
- Asking the Right Questions: Beyond the standard questions about symptoms, GPs delve deeper, inquiring about the patient's life circumstances, relationships, stressors, and coping mechanisms.
- Holistic Assessment: Moving beyond a focus on symptoms, GPs take a holistic approach, considering the patient's physical, emotional, social, and spiritual well-being.
- Providing Education and Support: GPs provide patients with accurate information about depression, its causes, and its treatment options. They also offer encouragement and support, reminding patients that they are not alone and that recovery is possible.
The Shocking Truth: Treatment Beyond the Prescription
While medication undoubtedly plays a vital role in treating many cases of depression, the "shocking secret" is that effective treatment often extends far beyond the prescription pad. Leading-edge GPs are increasingly emphasizing non-pharmacological interventions, recognizing the multifaceted nature of the illness.
Here are some key approaches:
- Psychotherapy: Cognitive Behavioral Therapy (CBT) and other forms of therapy are proven to be effective in treating depression. GPs can refer patients to therapists or, in some cases, provide brief counseling themselves.
- Lifestyle Modifications: Encouraging patients to adopt healthy habits, such as regular exercise, a balanced diet, sufficient sleep, and stress management techniques, can significantly improve their mood.
- Social Support: GPs can help patients connect with support groups, community resources, or other social networks that can provide a sense of belonging and reduce feelings of isolation.
- Mindfulness and Meditation: Cultivating mindfulness and practicing meditation can help patients manage stress, reduce negative thoughts, and improve their emotional regulation.
- Addressing Underlying Medical Conditions: GPs screen for other medical conditions, such as thyroid problems or vitamin deficiencies, that can contribute to depressive symptoms. They also adjust all other medications that may be leading to the patient's depression.
The Path Forward: A Call to Action for Patients and Healthcare Professionals
The fight against depression is far from over, but the insights gained from GPs provide a critical roadmap for the future. We must continue to break down the stigma surrounding mental illness, to empower individuals to seek help, and to ensure that healthcare professionals have the resources and training they need to provide effective care.
Here's how we can collectively make a difference:
- Patients:
- Acknowledge your feelings and seek help if you are struggling.
- Be honest with your GP about your symptoms and concerns.
- Follow your doctor's recommendations and actively participate in your treatment.
- Don't be afraid to ask questions and express your needs.
- Healthcare Professionals:
- Prioritize mental health awareness and training.
- Create a welcoming and supportive environment for patients.
- Take a holistic approach to diagnosis and treatment.
- Continuously seek to improve your knowledge and skills.
- Society:
- Reduce the stigma surrounding mental illness by promoting education and open dialogue.
- Advocate for increased funding for mental health services.
- Support initiatives that promote mental well-being in schools, workplaces, and communities.
The Takeaway: Embracing the Complexity and Finding Hope
The "shocking secret" about depression isn't a single revelation; it's the multifaceted understanding that emerges when we look beyond the surface. GPs, with their dedication, expertise, and unwavering commitment to their patients, are at the forefront of this journey. By embracing the complexity of the illness, fostering a culture of empathy, and embracing comprehensive treatment approaches, we can collectively transform the landscape of mental health and offer hope to those who need it most.
