Title: Depression Disorders in the DSM 5 TR Symptoms and Diagnosis
Channel: Doc Snipes
Depression Disorders in the DSM 5 TR Symptoms and Diagnosis by Doc Snipes
depressive disorders in dsm 5, depressive disorders in dsm 5 tr, mood disorders in dsm 5, mood disorders in dsm 5 tr, depression diagnosis in dsm 5, depressive disorders in children dsm 5, new depressive disorders in dsm 5, major depressive disorder in dsm 5, persistent depressive disorder in dsm 5, depressive disorders dsm 5 code
DSM-5 Depressive Disorders: The Shocking Truth Doctors Don't Want You to Know
Unmasking the Shadows: A Journey Through DSM-5 Depressive Landscapes
Depression. The word itself often carries a heavy weight, doesn't it? It’s a subject steeped in complexity and whispers of unspoken truths. We frequently hear about it. Nevertheless, do we truly grasp the multifaceted nature of depressive disorders, as outlined by the DSM-5? Let’s embark on a journey of discovery. We'll explore the terrain that many simply glance at.
Navigating the Labyrinth: What the DSM-5 Reveals
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is more than just a textbook. It's a comprehensive guide used by mental health professionals. It provides the current framework for understanding and diagnosing mental illnesses. The DSM-5 refines many classification nuances. Consequently, this allows for a more targeted approach to care. Depression, therefore, occupies a significant space. The DSM-5 doesn't only state facts. It organizes the vast spectrum of depressive disorders. Moreover, it defines the criteria for diagnosis.
Unpacking the Spectrum: Diverse Depressive Disorders
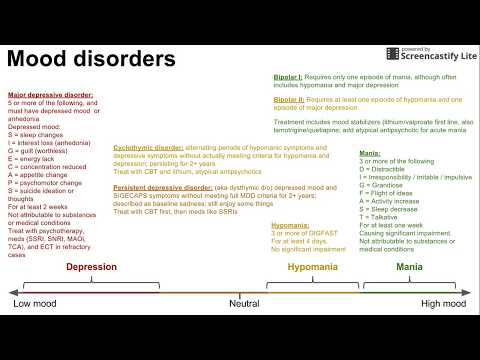
Depressive disorders aren't monolithic. Indeed, the DSM-5 recognizes a diverse range. Major Depressive Disorder (MDD) is perhaps the most widely recognized. It involves persistent feelings of sadness. Additionally, it has many other symptoms like loss of interest and fatigue. The severity and persistence of these symptoms characterize MDD. Persistent Depressive Disorder (Dysthymia) is present in many situations. This encompasses less severe, but chronic, depressive symptoms. Pre-Menstrual Dysphoric Disorder (PMDD) is another specific example. It specifically links depression to the menstrual cycle. Disruptive Mood Dysregulation Disorder (DMDD) shows itself in children. It is characterized by persistent irritability and frequent outbursts. These are but a few of the conditions acknowledged. The diversity reflects the complex interplay of factors causing depression.
Beyond the Diagnosis: Recognizing the Nuances
The DSM-5's value doesn't just rest in diagnosis. It helps understand the various manifestations of depression. Diagnostic criteria are essential tools for clinicians. However, it also emphasizes the importance of individual experience. Therefore, factors like cultural context, personal history, and physical health are crucial. The DSM-5 urges clinicians to embrace a holistic approach. This acknowledges the uniqueness of each individual's journey. Moreover, it encourages a personalized treatment plan. This often involves psychotherapy, medication, or a combination of both.
Early Detection: A Crucial First Step
Early detection dramatically improves outcomes. Recognizing the initial signs of depression is essential. In other words, awareness is paramount. Changes in sleep patterns, appetite fluctuations, and feelings of hopelessness are potential red flags. Besides, persistent fatigue, difficulty concentrating, and withdrawal from social activities are other symptoms. Seeking professional help is vital. Early intervention can prevent the condition from worsening. Furthermore, it can help people regain their quality of life. The DSM-5 plays an important role. It offers diagnostic clarity and empowers conversations.
The Ongoing Evolution: Modernizing Approaches
The field of mental health continues to evolve. Research continually refines our understanding of depression. Scientists constantly investigate new treatments and approaches. The DSM-5 is not a static document. Its guidelines are often updated, considering new evidence. Therefore, the dialogue about mental health is constantly changing. This makes mental health research a dynamic process. Thus, researchers continue to explore the genetic, environmental, and social factors. The aim is to refine treatment strategies. The goal is to improve patient outcomes.
Hope for Tomorrow: Embracing Compassion & Understanding
Depression is a challenging condition. It affects millions worldwide. It is not a sign of weakness. It’s a complex interplay of factors. The DSM-5 gives a structure to this complexity. With proper diagnosis and treatment, recovery is possible. Consequently, this also requires societal compassion and understanding. Let's commit to breaking down stigmas. Moreover, let’s prioritize mental health awareness. Encouraging open conversations about mental well-being is vital. Together, we can create a supportive environment. This allows people to seek help without fear.
Pregnant & Depressed? You're NOT Alone (Shocking Statistics Inside!)DSM-5 Depressive Disorders: The Shocking Truth Doctors Don't Want You to Know
Hey everyone, let's dive into something that affects millions, yet is often shrouded in mystery and, frankly, a bit of a cover-up: DSM-5 Depressive Disorders. We're going to pull back the curtain and expose some uncomfortable truths that, well, let's just say your doctor might not be telling you. Prepare for a wild ride!
1. The Iceberg's Tip: What We Think We Know About Depression
We all think we know what depression is, right? Sadness, feeling down, maybe a bit of world-weariness? That’s the iceberg’s tip. The reality, as outlined in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), is a tempest beneath the surface. The DSM-5, the bible of mental health diagnoses, lays out the criteria for various depressive disorders. It’s complex, nuanced, and, frankly, often oversimplified in everyday conversation. It's like trying to understand a symphony by listening to a single note.
2. The DSM-5: Your Handbook to the Mental Maze
So, what exactly is the DSM-5? Think of it as a giant, meticulously organized catalog of mental health conditions. It provides specific criteria for diagnosing everything from depression to schizophrenia. It’s a tool for doctors, therapists, and researchers. But here’s where things get tricky: relying solely on the DSM-5 can be like navigating a maze blindfolded. We need to understand its limitations.
3. Major Depressive Disorder: More Than Just a Bad Day
The big kahuna of depressive disorders is Major Depressive Disorder (MDD). This isn’t just a bout of the blues. MDD involves persistent sadness, loss of interest in activities you once loved, changes in appetite and sleep, fatigue, difficulty concentrating, and even thoughts of self-harm or suicide. The DSM-5 outlines specific criteria – you need to experience at least five of these symptoms for a minimum of two weeks to be diagnosed with MDD. Sounds simple, right? Not quite.
4. The Medication Merry-Go-Round: Are Pills Always the Answer?
Here's a truth bomb: medication is often the first line of defense. Antidepressants can be life-saving, no doubt. But, and this is a HUGE "but," they're not a magic bullet. They don’t work for everyone, and they come with side effects. And here's the kicker – frequently, doctors don't fully explain those. It's like being handed a map without a compass. We've got to look deeper and consider other options.
5. Beyond the Pill: Exploring Alternative Treatments
Thankfully, the world isn’t just pills and more pills. We're talking about therapy (cognitive behavioral therapy, interpersonal therapy – the list goes on!), lifestyle changes (exercise, diet, sleep hygiene), and even alternative therapies like acupuncture or mindfulness. Finding the right approach often involves trial and error, a journey of self-discovery. Think of it as assembling a puzzle; you need a variety of pieces to see the whole picture.
6. The Stigma Struggle: Why Silence Still Reigns
Let's be real: talking about depression is still tough. There’s a lingering stigma that makes people feel ashamed, weak, or like they should "just snap out of it." This stigma is a barrier to seeking help and prevents open conversations. It's like trying to fix a leaky pipe while pretending there isn't water everywhere.
7. The Impact on Daily Life: Depression's Grip
Depression doesn’t just stay in your head. It impacts every facet of your life: work, relationships, hobbies, even basic self-care. It's like a thick fog, blurring everything and making it hard to function. The DSM-5 acknowledges this but the holistic reality can often be overshadowed.
8. The Hidden Faces of Depression: A Palette of Illnesses
Depression isn't a one-size-fits-all experience. It comes in many forms, often masked by other conditions. These include:
- Persistent Depressive Disorder (Dysthymia): A chronic, low-grade depression. Think of it as a constant drizzle instead of a downpour.
- Premenstrual Dysphoric Disorder (PMDD): Severe mood changes, irritability, and other symptoms linked to the menstrual cycle.
- Seasonal Affective Disorder (SAD): Depression linked to changes in seasons, often triggered by lack of sunlight.
- Disruptive Mood Dysregulation Disorder (DMDD): Chronic, severe irritability and temper outbursts in children (a controversial addition to the DSM-5).
9. The Role of Biology: Are We Born This Way?
Genetics, brain chemistry, and hormones all play a role in depression. Certain genes may increase your risk, and imbalances in neurotransmitters like serotonin and dopamine are often implicated. But it’s not a simple equation; it’s a complex interplay of nature and nurture. Your brain is an intricate machine, and sometimes, it needs a tune-up.
10. Trauma's Shadow: The Link Between Past and Present
Childhood trauma, abuse, neglect – these experiences can significantly increase the risk of developing depression later in life. Unresolved trauma can warp your view of the world and your sense of self. It's like carrying a heavy backpack from your past, weighing you down in the present.
11. The Importance of a Holistic Approach: Mind, Body, and Soul
Treating depression shouldn’t just be about medication. It's about addressing the whole person: your mind, your body, and your spirit. This might involve therapy, lifestyle changes, social support, and even things like meditation or spending time in nature. It's a multi-pronged attack.
12. When to Seek Help: Recognizing the Red Flags
Don't wait until things get unbearable. If you're experiencing persistent symptoms of depression – sadness, loss of interest, changes in sleep or appetite – seek help. Don't be afraid to talk to your doctor, therapist, or a trusted friend or family member. It's okay to not be okay.
13. The Patient-Doctor Divide: Why Honest Communication Matters
Sometimes, there’s a disconnect between what doctors know and what they tell patients. Doctors are busy, and time is often limited. You have to be your own advocate. Ask questions, be honest about your symptoms, and don’t be afraid to seek a second opinion. This is your health.
14. Navigating the System: Finding the Right Resources
Finding the right treatment and support can feel overwhelming. Research local therapists, support groups, and mental health organizations. Use online resources (but always vet them!) and don’t give up if the first option isn’t a good fit. It's a marathon, not a sprint.
15. The Future of Mental Health: Hope on the Horizon
Research is constantly evolving. New treatments and therapies are being developed, and the conversation around mental health is slowly, but surely, becoming more open. We're on the cusp of a mental health revolution. The future is filled with hope.
Closing Thoughts:
Depression is a complex beast, and the DSM-5 provides a framework for understanding its many faces. But remember, it's just a framework. The truly "shocking truth" is that so much remains misunderstood. It's up to us, as individuals and as a society, to keep the conversation going, to challenge the stigma, and to advocate for better care. Don't be afraid to seek help, to ask questions, and to fight for your mental well-being. You are not alone.
Frequently Asked Questions (FAQs):
1. What causes depression?
Depression is likely caused by a combination of factors, including genetics, brain chemistry, hormones, stressful life events, and personality traits. It's rarely just one thing.
2. How is depression diagnosed?
Diagnosis typically involves a mental health professional assessing your symptoms and history. They'll use the DSM-5 criteria as a guide. This often involves a physical exam to rule out any underlying medical conditions.
3. Are there different types of depression?
Yes! The DSM-5 outlines several depressive disorders, including Major Depressive Disorder, Persistent Depressive Disorder (Dysthymia), Seasonal Affective Disorder (SAD), and others.
4. How is depression treated?
Common treatments include medication (antidepressants), therapy (such as cognitive behavioral therapy or interpersonal therapy), lifestyle changes (exercise, diet, sleep hygiene), and alternative therapies (acupuncture, mindfulness).
5. Can I take an online test to diagnose myself?
Online quizzes can give you an idea if you might have depression, but they are not a substitute for professional diagnosis. Always consult with a healthcare provider for an accurate assessment.
1) Principal Keywords: DSM-5 Depression Truths Doctors 2) SEO Headline: Shocking Truths: DSM-5 Depressive Disorders Revealed 3) Pathway: DSM-5 Truth 4) Meta Summary: Uncover the shocking truths about DSM-5 depressive disorders. Discover what doctors might not tell you. Learn about medication, therapy, stigma, and more. 5) Image Alt Text: A fractured
Is THIS Depression? (Secret Unblocked Test)Depressive Disorders Intro Psych Tutorial 236

By PsychExamReview Depressive Disorders Intro Psych Tutorial 236 by PsychExamReview
Depressive and Bipolar Disorders Crash Course Psychology 30

By CrashCourse Depressive and Bipolar Disorders Crash Course Psychology 30 by CrashCourse
Title: Mood disorders depression, maniabipolar, everything in between
Channel: MedLecturesMadeEasy
Mood disorders depression, maniabipolar, everything in between by MedLecturesMadeEasy
Escape the Darkness: Your Guide to Overcoming Depression
DSM-5 Depressive Disorders: Unveiling the Complexities and Reclaiming Your Narrative
We understand the weight you carry. The silent struggles, the internal battles, and the persistent shadows that seem to darken your days. We also understand the frustration that can arise when seeking clarity about your mental health. The diagnosis of a depressive disorder, outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), can feel overwhelming. The sheer volume of information, coupled with the unique nuances of each individual’s experience, can make navigating this landscape feel like traversing an uncharted territory. Our goal is to illuminate the path, offering a guide that transcends generic explanations, providing a deep dive into the DSM-5 criteria, and empowering you to reclaim control over your life.
Demystifying the DSM-5: A Framework for Understanding
The DSM-5, a publication of the American Psychiatric Association, is the guidebook clinicians use to diagnose mental disorders. It provides a common language for mental health professionals, ensuring consistency in diagnosis and treatment. However, the complex nature of depressive disorders requires a more profound understanding of the DSM-5 framework.
The DSM-5 recognizes several depressive disorders, each with its unique characteristics, diagnostic criteria, and treatment approaches. Understanding these distinct presentations is essential for accurate diagnosis and tailored intervention.
Major Depressive Disorder: Beyond the Blues
Major Depressive Disorder (MDD) is perhaps the most commonly recognized form of depression. It's characterized by at least two weeks of persistent low mood or loss of interest or pleasure, along with at least five of the following symptoms:
- Depressed mood: Feeling sad, empty, or hopeless most of the day, nearly every day.
- Loss of interest or pleasure: Diminished interest or pleasure in activities that were once enjoyable.
- Significant weight loss or gain: A noticeable change in weight or appetite (e.g., eating much more or less than usual).
- Insomnia or hypersomnia: Difficulty sleeping or sleeping excessively.
- Psychomotor agitation or retardation: Restlessness or slowed movements and speech.
- Fatigue or loss of energy: Feeling tired or drained most of the day.
- Feelings of worthlessness or excessive guilt: Negative self-perceptions, often involving blame or feelings of inadequacy.
- Difficulty concentrating or making decisions: Problems focusing, remembering, or making choices.
- Recurrent thoughts of death or suicide: Thinking about death, suicide, or having a suicide plan.
It's important to understand that the presence of these symptoms alone doesn't automatically equate to an MDD diagnosis. The DSM-5 requires that the symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning. Furthermore, the symptoms must not be attributable to the physiological effects of a substance or another medical condition. The experience varies drastically from person to person, which further proves the necessity of seeking professional evaluation.
Persistent Depressive Disorder (Dysthymia): A Chronic Low
Persistent Depressive Disorder, formerly known as dysthymia, is characterized by a chronically depressed or irritable mood. The duration of this low mood must be for at least two years in adults (or one year in adolescents and children). While the intensity of the symptoms may fluctuate, the depressed mood is usually present most of the day, for most days. Along with depressed mood, individuals with Persistent Depressive Disorder must exhibit at least two of the following:
- Appetite changes.
- Sleep disturbances (insomnia or hypersomnia).
- Fatigue or low energy.
- Low self-esteem.
- Difficulty concentrating or making decisions.
- Feelings of hopelessness.
Unlike MDD, Persistent Depressive Disorder allows for periods of respite but these periods are generally brief, lasting no more than two months.
Premenstrual Dysphoric Disorder (PMDD): A Cyclical Struggle
Premenstrual Dysphoric Disorder (PMDD) is a severe form of premenstrual syndrome (PMS) that significantly impacts mood and functioning in the days or weeks leading up to menstruation. This involves marked mood lability (e.g., mood swings; feeling suddenly sad or tearful, or increased sensitivity to rejection), marked irritability or anger or increased interpersonal conflicts, depressed mood, feelings of hopelessness, or self-deprecating thoughts, and anxiety.
To be diagnosed with PMDD, at least five symptoms must be present in the final week before the onset of menses, improve within a few days after menses onset, and be minimal or absent in the week after menses. These symptoms include affective lability; irritability or anger; depressed mood, hopelessness, or self-deprecating thoughts; anxiety, tension, and/or feeling on edge; decreased interest in usual activities; difficulty concentrating; lethargy, easy fatigability, or marked lack of energy; change in appetite; hypersomnia or insomnia; feeling overwhelmed or out of control; and physical symptoms, such as breast tenderness or bloating. A thorough intake and documentation of these symptoms are required to accurately diagnose this disorder.
Disruptive Mood Dysregulation Disorder (DMDD): Recognizing Childhood Challenges
Disruptive Mood Dysregulation Disorder (DMDD) is a condition characterized by chronic, severe irritability and anger in children and adolescents. This condition is categorized by frequent temper outbursts that are inconsistent with the child's developmental level. These outbursts are typically verbal and/or behavioral (e.g., physical aggression toward people or property), and they occur on average three or more times per week. The mood between outbursts is persistently angry or irritable most of the day, nearly every day, and is observable by others (e.g., parents, teachers, peers). The diagnosis of DMDD is only given to children and adolescents aged six to 18 years.
Other Specified Depressive Disorder and Unspecified Depressive Disorder: Recognizing the Gray Areas
Sometimes, the Diagnostic and Statistical Manual does not fit. There are cases where symptoms of a depressive disorder are present but do not fully meet the criteria for any of the specific disorders. In these instances, a clinician may use the "Other Specified Depressive Disorder" or "Unspecified Depressive Disorder" diagnoses. "Other Specified Depressive Disorder" is used when the clinician can specify the reason why the criteria for MDD or other depressive disorders are not met (e.g., short-duration depressive episode). "Unspecified Depressive Disorder" is used when the clinician does not want to specify the reason for not meeting the criteria.
Beyond the Diagnosis: Embracing a Holistic Approach
Understanding the diagnostic criteria is only the first step. The journey towards healing and well-being encompasses a multifaceted approach, including treatment options and lifestyle adjustments.
- Therapy: Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT), and psychodynamic therapy are just a few of the therapeutic approaches that can be highly effective in managing depressive symptoms and developing coping mechanisms.
- Medication: Antidepressants, prescribed by a medical professional, can help regulate brain chemistry and alleviate symptoms. A thorough discussion with your doctor about potential benefits, side effects, and interactions is essential.
- Lifestyle modifications: Regular exercise, a balanced diet, sufficient sleep, and stress-reduction techniques (e.g., mindfulness, meditation) can significantly impact both physical and mental health.
- Social Support: Connecting with supportive friends, family, or support groups can provide invaluable emotional support.
Finding Your Path to Recovery
The diagnosis and treatment of depressive disorders are unique for each individual. There are no shortcuts. The key is to be proactive, informed, and compassionate with yourself throughout the process. Consider the following:
- Seek professional guidance: Consult with a qualified mental health professional for an accurate diagnosis and personalized treatment plan.
- Educate yourself: Read credible resources and seek information from reputable organizations. Expand your knowledge and deepen your understanding.
- Prioritize self-care: Incorporate activities that bring you joy and relaxation. Nurture your mind, body, and spirit.
- Build a support system: Connect with loved ones or join a support group. Share your experiences and receive support from others.
- Advocate for yourself: Communicate your needs and concerns to your healthcare providers. Actively participate in your treatment plan.
- Be patient: Recovery takes time. Celebrate your progress and show yourself grace during setbacks. Be kind to yourself.
You are not alone. You are not defined by your diagnosis. You have the strength to overcome the challenges of depressive disorders and reclaim your life. Empower yourself. Seek help. Believe in your ability to heal. The road ahead may not be easy, but you are worthy of support, understanding, and a life filled with joy. Take the first step. Reach out. Start your journey today.